Stroke Fact Sheet
CIRM funds many projects seeking to better understand stroke and to translate those discoveries into new therapies.
Description
In the U.S., almost 800,000 people have a stroke each year and more than 140,000 people die of their stroke. It is the leading cause of serious, long-term disability in the U.S.
Stroke occurs when a blood clot blocks a vessel in the brain and cuts off blood flow. Brain cells begin to die within minutes when they are deprived of oxygen and nutrients. A less common kind of stroke involves a burst blood vessel that bleeds into the brain, also killing brain cells. Losing these brain cells can cause permanent problems with movement and cognitive abilities such as memory, attention span even speaking or understanding speech.
A stroke requires immediate treatment. Signs of stroke include sudden onset of numbness of the face, arm or leg, confusion, blurred vision, dizziness or headache. Doctors can intervene by dissolving the clot and restoring blood flow or stopping the bleeding.
After a stroke, intensive physical therapy can help people regain some lost function. However, there is currently no therapy to restore the brain cells that have died as a result of the stroke.
Stem cell scientists are attempting to use different types of stem cells including tissue-specific neural stem cells, embryonic stem cells and reprogrammed iPS cells to replace cells lost during a stroke. They are testing the different cell types in animal models of stroke to see which are best able to restore movement. They also need to learn the best way of delivering those cells into the brain. Around the country, several clinical trials are underway testing different type of cells and different delivery methods. Other researchers are seeing if it’s possible to activate the stem cells in the brain to repair the damage.
CIRM Grants Targeting Stroke
| Researcher Name | Institution | Grant Title | Grant Type | Award Amount |
| Dr. Yadong Huang | Gladstone Institutes, J. David | Defining the Isoform-Specific Effects of Apolipoprotein E on the Development of iPS Cells into Functional Neurons in Vitro and in Vivo | New Faculty II | $2,757,303 |
| Dr. Stuart A Lipton | Sanford Burnham Prebys Medical Discovery Institute | MEF2C-Directed Neurogenesis From Human Embryonic Stem Cells | Comprehensive Grant | $2,832,000 |
| Dr. Samuel Pleasure | University of California, San Francisco | Human stem cell derived oligodendrocytes for treatment of stroke and MS | Comprehensive Grant | $2,459,235 |
| Dr. Guoping Fan Dr. | University of California, Los Angeles | Epigenetic gene regulation during the differentiation of human embryonic stem cells: Impact on neural repair | Comprehensive Grant | $2,412,995 |
| Professor Ziwei Huang | Sanford Burnham Prebys Medical Discovery Institute | New Chemokine-Derived Therapeutics Targeting Stem Cell Migration | SEED Grant | $708,000 |
| Dr. Gary Steinberg | Stanford University | Embryonic-Derived Neural Stem Cells for Treatment of Motor Sequelae following Sub-cortical Stroke | Disease Team Research I | $17,244,851 |
| Irene Lorenzo Llorente | Palo Alto Veterans Institute for Research | Inhibitory interneurons derived from human induced pluripotent stem cells to treat stroke | Quest – Discovery Stage Research Projects | $2,140,122 |
| Dr. Thomas Carmichael M.D., Ph.D. | University of California, Los Angeles | Human-induced pluripotent stem cell-derived glial enriched progenitors to treat white matter stroke and vascular dementia. | Quest – Discovery Stage Research Projects | $250,000 |
| Dr. Thomas Carmichael M.D., Ph.D. | University of California, Los Angeles | iPS Glial Therapy for White Matter Stroke and Vascular Dementia | Quest – Discovery Stage Research Projects | $2,086,130 |
| Dr. Thomas Carmichael M.D., Ph.D. | University of California, Los Angeles | iPS-Interneuron Transplantation for Neural Repair after Stroke | Inception – Discovery Stage Research Projects | $229,396 |
| Irene Lorenzo Llorente | Palo Alto Veterans Institute for Research | Clinical Translation of Allogenic Regenerative Cell Therapy for White Matter Stroke and Vascular Dementia | Therapeutic Translational Research Projects | $5,149,913 |
| Dr. Irene L. Llorente | University of California, Los Angeles | Clinical Translation of Allogenic Regenerative Cell Therapy for White Matter Stroke and Vascular Dementia | Therapeutic Translational Research Projects | $707,754 |
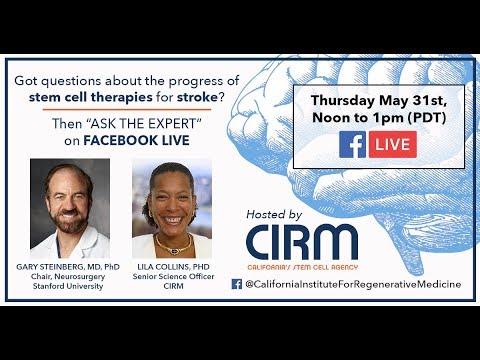
| Dr. Gary Steinberg | Stanford University | Safety and Tolerability Study of Neural Stem Cells (NR1) in Subjects with Chronic Ischemic Subcortical Stroke | Clinical Trial Stage Projects | $11,998,988 |
| Dr. Bijan Nejadnik | SanBio, Inc. | A Double-Blind, Controlled Ph 2b Study of the Safety and Efficacy of Modified Stem Cells in Patients with Chronic Motor Deficit from Ischemic Stroke | Clinical Trial Stage Projects | $18,970,000 |
| Dr. Gary Steinberg | Stanford University | Intraparenchymal NR1 Stem Cell Therapy for Chronic Subcortical Ischemic Stroke | Late Stage Preclinical Projects | $5,300,000 |
| Dr. Gary Steinberg | Stanford University | Paracrine and synaptic mechanisms underlying neural stem cell-mediated stroke recovery | Basic Biology V | $1,178,370 |
| Dr. Stuart A Lipton | The Scintillon Institute | Programming Human ESC-derived Neural Stem Cells with MEF2C for Transplantation in Stroke | Early Translational IV | $1,103,185 |
| Dr. Stuart A Lipton | Sanford Burnham Prebys Medical Discovery Institute | Programming Human ESC-derived Neural Stem Cells with MEF2C for Transplantation in Stroke | Early Translational IV | $1,020,815 |
| Dr. Brian K. Rutt | Stanford University | Development of Single Cell MRI Technology using Genetically-Encoded Iron-Based Reporters | Tools and Technologies II | $1,833,348 |
| Dr. Thomas Carmichael M.D., Ph.D. | University of California, Los Angeles | Development of a Hydrogel Matrix for Stem Cell Growth and Neural Repair after Stroke | Tools and Technologies II | $1,825,613 |
| | | | Total:
$82,208,017.07 |
CIRM Stroke Videos
News and Information
Resources
Find Out More:
Stem Cell FAQ | Stem Cell Videos | What We Fund